If you’ve been trying to lose weight with the help of modern medication, you may have already noticed it’s not as simple as booking a GP appointment.
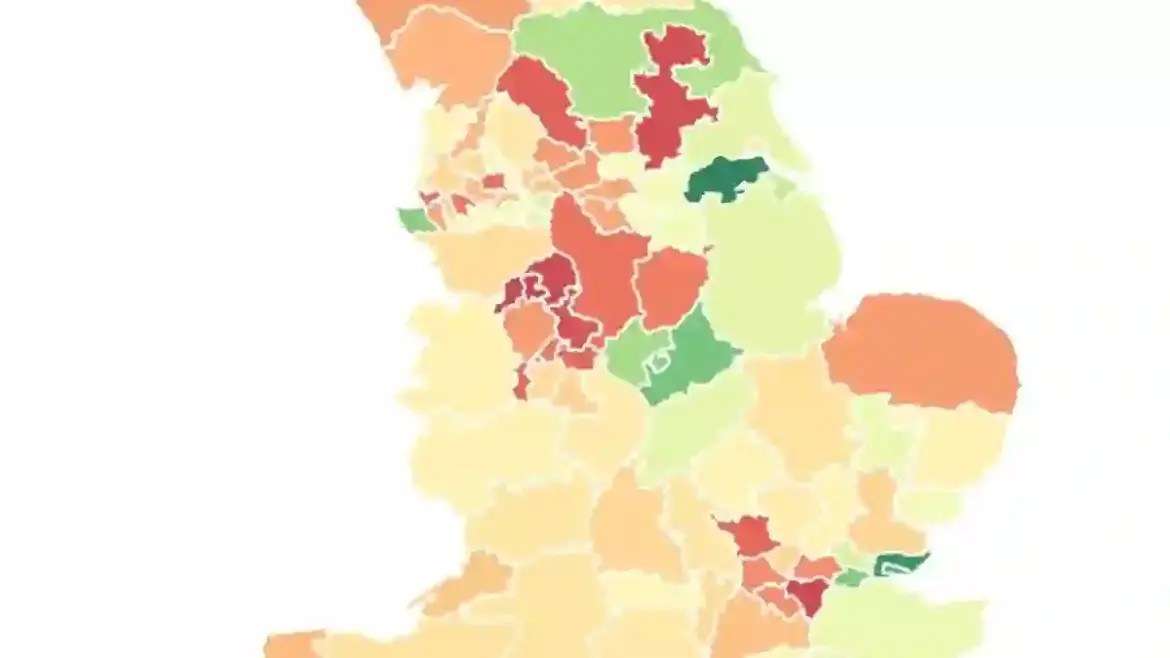
Across England, access to slimming injections like Mounjaro and Wegovy is patchy at best, with some areas being well-stocked while others are almost completely empty.
Experts are now warning that this “postcode lottery” is leaving millions of overweight adults without vital treatments.
Prescription Gaps Highlight Regional Inequality
New data shows huge discrepancies in who can actually get these drugs on the NHS.
In North Lincolnshire, June figures revealed 2,445 prescriptions for GLP-1 injections – the category these appetite-suppressing drugs fall under.
That works out to about 1,250 prescriptions for every 10,000 obese adults.
Meanwhile, North Tyneside, one of the nation’s biggest “black spots,” recorded just 265 per 10,000.
With supplies costing roughly £3,000 per year per patient, many people are forced to pay privately, with some high street pharmacies charging up to £200 a month.
Why the Rollout Is So Slow
The slow NHS rollout is partly down to cost and partly to logistics.
Health watchdogs have been cautious, fearing GP practices could be overwhelmed.
Current estimates suggest it could take up to 12 years to offer these injections to all 3.4 million eligible patients under NHS criteria.
Experts argue this leaves hundreds of thousands without support, driving a booming private market for those who can afford it.
Professor Nick Finer, a leading obesity researcher, said: “It is truly a postcode lottery.
It’s extraordinary the NHS has been so slow to deliver these drugs to people who need them.”
Government Seeks to Accelerate Access
Ministers are keen to speed things up. Keir Starmer has described GLP-1 drugs as potentially “very important for our economy,” while Health Secretary Wes Streeting suggested they could help obese unemployed people return to work.
Despite this, NHS prescribing data does not reveal whether the drugs were used for type 2 diabetes or weight loss, complicating the picture.
How GLP-1 Injections Work
GLP-1 injections, such as Mounjaro, Wegovy, and Saxenda, work by suppressing appetite, making the brain feel full and reducing overeating.
They have proven highly effective, but their cost and limited supply have created unequal access.
The NHS prioritizes patients with multiple weight-related health problems, often requiring them to attend specialist Tier 3 weight-management clinics.
Private Market and Misuse
Because NHS supply is limited, private prescriptions now dominate, with estimates suggesting they account for 90% of GLP-1 usage.
Some people have even misrepresented their weight to online pharmacies to gain access, leading to hospital admissions for side effects.
A surge in demand recently forced the US manufacturer of Mounjaro to impose a temporary UK-wide freeze on orders, with prices set to increase from £122 to £330 per month for the highest dose.
Experts Warn About Two-Tier System
The rapid private market expansion has created what experts call a “two-tier system,” worsening health inequalities.
Obesity rates are roughly 15% higher in the most deprived areas, and those who cannot pay for private treatment are left behind.
Think tanks warn this could disproportionately harm people with learning disabilities or severe mental illnesses, who need more personalized care.
Looking to the Future
Pharmaceutical competition may soon bring more affordable versions of these drugs.
For instance, patents for semaglutide (Ozempic and Wegovy) are set to expire in 2026 in some regions, which could lower costs.
Meanwhile, the NHS is scaling up new services to provide weight-loss support safely and effectively, starting with the patients who are most in need.
Professor Finer added: “When artificial hips came out, millions qualified.
It took time to roll them out. GLP-1 drugs are similar – a slow, careful rollout is realistic, but the goal should be universal access.”
The Urgent Need to Tackle Obesity
Obesity in the UK is not just a cosmetic concern – it has real consequences for health and life expectancy.
Life expectancy has dropped, hospital admissions for weight-related conditions are rising, and the NHS spends billions annually addressing obesity-related illnesses.
Experts agree that while drugs are transformative, prevention and lifestyle support remain vital to tackle the crisis effectively.
An NHS spokesman concluded: “Weight-loss drugs have a vital role in helping people manage their weight and lead healthier lives.
We are rolling out lifestyle and medical support to ensure equitable access for all eligible patients as part of holistic care.”